 Frill is a term that is used by patients who have had an FOV (Vitrectomy for Floaters) to describe a visual disturbance that occasionally occurs post-operatively in their peripheral (side) vision. This “frill” is noted by a very small subset of patients who have undergone a successful vitrectomy for floaters (FOV), that is, the floaters have been successfully removed, but a secondary problem has developed in the peripheral vision.
Frill is a term that is used by patients who have had an FOV (Vitrectomy for Floaters) to describe a visual disturbance that occasionally occurs post-operatively in their peripheral (side) vision. This “frill” is noted by a very small subset of patients who have undergone a successful vitrectomy for floaters (FOV), that is, the floaters have been successfully removed, but a secondary problem has developed in the peripheral vision.
Unfortunately, I am unable to see “frill” through a visual examination of a patient. Nonetheless, I do sympathize with those patients who experience “frill.”
Moreover, since “frill” has not been medically defined there is no specific course of treatment.
Goal of Vitrectomy for Floaters
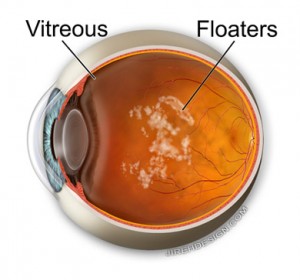
The goal of performing a vitrectomy for floaters is to remove and significantly reduce the number of floaters, and to do it safely. Infection, retinal tears/detachment and cataract formation are the major complications which must be considered for every patient who requires a vitrectomy, regardless of cause.
The practice of medicine is inexact and no two patients are exactly the same. Prior to obtaining a patients consent to perform a vitrectomy for the removal of floaters, I always advise that surgery may not remove all of the floaters. I do not use the term “frill” in my consent because it is not a medical term, however, I do note that residual floaters may remain.
Safety is also a goal of every surgery. I want to remove as much vitreous as possible without damaging the retina; therefore, all of the vitreous is not removed. I do this by removing the central “core” of the vitreous. The depth and the amount removed to the sides is not an exact science. I remove what I believe is a safe amount without compromising the retina. Remember, this can and will vary patient to patient.
Frill is Not a Complication of Vitrectomy
For reasons that I do not know, a small subset of patients who undergo vitrectomy report post-operatively a different type of visual disturbance than the floaters. Fortunately, while still bothersome, the disturbances are noted in their peripheral vision.
And for those few who feel they cannot function due to the peripheral abnormalities, the only recourse may be to recommend a second surgery to remove additional vitreous. With each surgery though there are risks, so the risk/benefit ratio must be fully appreciated by patients wishing to entertain a second surgery.
If I were a medical researcher with the facilities and budget to explore “frill” and its causes I certainly would; however, I am not a researcher. Instead, I use the tools and research of others to best help those in need. At this point, for patients who have had their daily activities compromised by floaters, I recommend a vitrectomy to remove the floaters.
What Does This Mean?
My goal in performing an FOV or vitrectomy for floaters, is to restore a patient’s ability to function in their daily activities without be hindered by debilitating floaters in their central vision. Over 22 years, I have performed thousands of vitrectomies and out of all of those vitrectomies only four patients have reported “frill.”
I do not say this to dismiss the very, real complaint of additional visual disturbances, rather, to show why I still believe that for the vast majority of patients I treat, vitrectomy is a highly effective procedure and that “frill” does not occur most of the time…making it even more difficult to figure out why it develops.
I understand that “frill” is discussed widely on forums and, for those patients, it is extremely frustrating to have undergone surgery, yet be left with a visual disturbance in their peripheral vision. The following possibilities are what I believe could explain post-operative “frill” and would be happy to discuss further (in later posts) with anyone who is in an ophthalmic research position that would like to explore these possible causes in greater detail.
- Unremoved Vitreous
- Shifting Vitreous
- Changing Vitreous
- Relative Loss
- Vitreous Hydration
Randall V. Wong, M.D.
Ophthalmologist, Retina Specialist
Fairfax, Virginia
Randall V. Wong, M.D.
Ophthalmologist, Retina Specialist
Fairfax, Virginia
***This post is for information purposes only. This posting does not offer legal or medical advice, so nothing in it should be construed as legal or medical advice. The information on this blog/post is only offered for informational purposes. You shouldn’t act or rely on anything in this blog or posting or use it as a substitute for legal/medical advice from a licensed professional. The content of this posting may quickly become outdated, especially due to the nature of the topics covered, which are constantly evolving. The materials and information on this posting/blog are not guaranteed to be correct, complete, or timely. Nothing in this posting/blog and nothing you or I do creates a doctor-patient relationship between you and the blog; between you and me; or between you and Randall Wong, M.D. or RetinaEyeDoctor.com. Even if you try to contact me through the blog or post a comment on the blog you are still not creating a doctor-patient relationship. Although, I am a doctor, I’m not YOUR doctor until and unless there is a written agreement specifically providing for a doctor-patient relationship.***