In the summer of 1990, my wife and I were invited to join a People to People Ambassador Tour to visit the Soviet Union. The USSR didn’t break up into its member states until the following year, late 1991. So, we got a look at what turned out to be a huge national facade – a strong military front and a “third world” infrastructure.
I was part of a medical group (medical laser specialists) that visited several hospitals and laser centers (?) within Moscow (Russia), Tbilisi (Soviet Georgia), Kharkov (Ukraine) and in St. Petersburg (again, in Russia). Fortunately, my wife was able to join up with a group of performing artists that were also on an Ambassador tour and, while we (the medical group) were doing our hospital visits, they visited their Soviet peers,.
For the record, Moscow was bleak, with the exception of our visit to the Kremlin, and the gift shopping – my wife got a beautiful amber necklace from a street vendor for $20, and I came back with a set of matryoshka (nesting) dolls, with Gorbachev on top and Lenin deep inside at the bottom). In contrast, Tbilisi in Soviet Georgia was colorful and hot (90 degrees when we were there). The Ukraine, our next stop, was the food basket of Russia, but because they had few refrigerated trucks, there was no way of moving the food into the cities! Our final stop was St. Petersburg (or Leningrad, whichever you prefer), which was beautiful. It is a land of rivers and bridges – and the Hermitage, the most beautiful museum that we have ever visited!
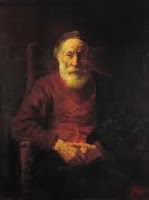
A brief anecdote – the day before our visit to the Hermitage, one of my colleagues ran out of 35 mm film and I gave him a couple of rolls of the 400 speed film that I was using. The next day, he replaced my rolls with a couple of rolls of 1000 speed film, which enabled me to take some beautiful pictures inside the Hermitage, including of the huge malachite urns and a couple of Rembrandt paintings (one of a man in a red coat – which I believe was a self-portrait, and Moses with his son Isaac on the mount) without needing to use a flash, which was forbidden inside the museum. I have included a few of these photos for your enjoyment – actually, the Rembrandt’s are from the web, as they are much better reproductions than I was able to achieve from my 35mm slides.)
We flew Aeroflot within the USSR – no seat belts, animals on board, and tea service served in cracked cups by heavy-set women with gold teeth! The planes were flown by military pilots, who were the first to get off, and the rear section of the plane was unloaded first to keep the planes balanced!
When we visited, most people worked for the state – and there wasn’t any work! So they would go to their jobs in the morning and, having nothing to do there, would be back on the streets by noon. It just goes to prove that the communist way of doing things didn’t work. There were no goods in the stores, and what we did see was both sparse and of poor quality (paper shoes?). And, long lines everywhere to get tobacco and vodka.
Based on my experiences, I published two articles about my trip; one about the state of healthcare (and lack of lasers) in the USSR, and a second on the state of eyecare in that part of the world. They are technical in nature but illustrate the differences between what the Soviet Union was telling the world and what we actually saw!
Here, for your further enlightenment, are the two articles I wrote about our (the medical groups’) experiences.
The State of Healthcare in the Soviet Union: The Lack of Medical Lasers
This article was published in both Medical Laser Industry Report, October 1990 and Laser Report, December 15, 1990.
Irving J. Arons
Arthur D. Little
During late July 1990, I was privileged to join a delegation of medical laser specialists and other health care professionals, under the auspices of the People to People Ambassador Program, invited to tour the medical community in the Soviet Union. Our group, organized by the American Society for Lasers in Medicine and Surgery, was composed of specialists in gynecology, plastic surgery, thoracic surgery, urology, general medicine, and myself, representing the field of ophthalmology. In addition to the ASLMS group, a veterinarian working with lasers, a health care safety specialist, and two medical technical/clinical lab specialists were included in our delegation.
We were able to visit a medical laser research institute in Moscow, and four hospitals, one each in Moscow (Soviet Russia), Tbilisi (Soviet Georgia), Kharkov (Soviet Ukraine), and Leningrad/St. Petersburg (Soviet Russia, again).
Our overall impression was that the facilities and equipment in use were woefully decrepit and/or non-existent or years behind Western standards. However, the medical personnel we met were dedicated professionals.
Of particular note, we found that the hospitals — even one claimed to be only three years old — were ill kept and falling apart. The facades were cracked and broken, the hallways and stairwells unswept, and the grounds surrounding the buildings not cared for at all. In counterpoint, we found the patient rooms were clean and staffed with dedicated nurses and doctors doing their best with what they had. This was particularly evident at the Karzigan Childrens Hospital in Moscow. The wards were filled with children with trauma of all kinds, but they were all smiling and very well cared for by an attentive staff of nurses and aides. It was here that we learned that a typical doctor with less than 10 years service earns between 240-260 rubles a month (the equivalent to about $40 at the official exchange rate of 6 rubles to the dollar, and only $20-30 at the black market exchange rate of 10-15 rubles to the dollar), a beginning research worker earns 140-150 rubles per month, and a surgical nurse get about 110 rubles for regular shifts. (In contrast, the bus drivers providing our transportation were paid 400 rubles/month and we were told that street sweepers earned as much as 700 rubles/month!)
The hospital equipment, especially for diagnosis and surgery, was particularly non-existent, and, according to our laboratory clinicians, the clinical laboratory equipment was barely adequate to care for the patients in the wards. But we must emphasize, both the hospital administration and medical staff were dedicated to providing the best care possible to their patients. What they lacked in equipment they more than made up with in numbers and dedication.
As for medical lasers, and new medical treatments using lasers, except for the laser institute in Moscow, the only lasers that the hospitals seemed to have were low powered therapeutic types, basically HeNes and GaAs infrared lasers. The hospital in Leningrad had several CO2 lasers, and claimed to have other surgical equipment, but we only saw therapeutic lasers in operation. We were told that only about 100 of approximately 15,000 hospital-based physicians in Kharkov have access to or use surgical lasers. We would guess that the percentages are not much different in the other 14 Soviet Republics. At the hospitals we visited, the majority of the half dozen lasers they claimed to have — if they had any — were either HeNe or GaAs therapy lasers, used to treat open sores, pain, and in one hospital in Tbilisi (Soviet Institute of Clinical & Therapeutical Research), for treating myocardial infarctions by clearing viruses in the blood through intravenous use of a HeNe laser connected to a fiber inserted through an arm vein. The same hospital also used a scanning HeNe laser to alleviate angina chest pain by scanning the laser beam across the patient’s chest!
At a trauma hospital in Leningrad (The Ambulatory Institute Hospital), we saw a 40-50 watt CO2 laser in the corner of an operating room, and another upstairs in a storeroom along with the usual HeNe lasers. We saw no evidence of a YAG laser although the laser specialist at this hospital claimed to have just received one, but which he had not yet unpacked. In the same storeroom with the spare CO2 laser, we were told that a small laser sitting on top of packing crates was a new UV laser, apparently solid-state since there was no evidence of any gas bottles or connections for one. (An interesting side note, we observed a burn therapy ward at this hospital, and it was disconcerting to see flypaper strips hanging from the ceiling.)
At the hospital in Kharkov (The Central Regional Hospital), we were told that they had an Ar laser used in ophthalmic treatments (but we did not see it).
The National Research Institute of Laser Surgery in Moscow claimed to be doing considerable research with medical lasers, performing 47,000 laser procedures annually. It is supposedly, one of 52 laser centers in the Soviet Union. We were given a presentation about the clinical research they were doing with five types of high power lasers, mostly CO2 and YAG — and two prototype free electron lasers, used for PDT studies. The FELs, according to the slides shown us, may be revolutionary, in that they appeared to be about the size of a large sized desk, much smaller than any other FEL I have seen — and I have seen the Stanford FEL and pictures of others. Attempts to find out more about this laser development were fruitless, however I plan to get back in touch with my contact at the Institute to see if I can possibly learn more about this exciting laser development. (Several weeks after my return to the States, I received a call telling me that a defector from the Moscow Laser Institute wanted me to know that he had built the laser in question and it was not an FEL, but rather an electron beam generator pumping a chemical laser use in their PDT work.) When we asked to see their lasers, we were politely told that they were in another building and couldn’t be shown to us. Apparently, the person holding the key to the lab was not available!
According to a profile of the Soviet healthcare community recently published by Medistat, a UK healthcare publication, what we saw in the Soviet Union this summer is typical and not out of line with what others have reported. The Medistat profile stated that the Soviet Union has some 23,000 hospitals with 3.6 million beds, and in addition, some 38,000 polyclinics and other outpatient centers. Capital investment in recent years has concentrated on the construction of new facilities to boost the number of beds, but many of the new facilities have been built at unsuitable sites, and the majority of Soviet hospitals having little in modern equipment with some lacking the basic necessities of adequate sanitary facilities or even heating.
The polyclinic is the main unit in the primary healthcare network, and the first point of contact for most Soviet patients. They serve districts of 50,000 to 60,000 inhabitants and are staffed by doctors responsible for around 2000 patients. In addition to general doctors, each polyclinic has specialists in area such as cardiovascular disease, oncology and renal medicine.
The Soviet Union has the highest number of doctors per capita, with a total of 1.3 million doctors serving a population of 275 million. In addition, there are 3.3 million medical assistants. Women doctors are well represented, accounting for about 70% of all doctors. (We were told the percentage was closer to 50%, at least at the facilities we visited.)
As you know, until recently, all planning was done centrally, and for five years in advance — the so called Five Year Plan. The most recent healthcare plan was put together in August 1987. That five-year plan attempted to address the chronic underfunding of the healthcare system, calling for new hospitals while neglecting older ones which will now need to undergo drastic major refurbishment. Expenditures for medical equipment had also been limited in the past, with the majority of funds allocated for new buildings. But the new policy included allocation of more resources for the purchase of modern equipment, in particular the polyclinic facilities were to be upgraded with proper diagnostic and treatment services to enable the patients to be treated at the clinic rather than to be referred to local hospitals. According to Medistat, 5.4 million rubles had been allocated for the purchase of new equipment over the two year period 1988-1989.
Discussing the state of the Soviet medical equipment market, Medistat states that the USSR suffers from a chronic shortage of equipment, particularly in the high tech areas such as computerized scanning, ultra-sound, renal equipment, and as we found out, laser treatment devices. Even basic equipment such as electrocardiographs and routine surgical instruments and disposable syringes are in short supply, with the problem being further aggravated by the fact that much of the Soviet produced equipment is sub-standard.
The current five-year plan envisages accelerating development in the medical industry and raising the technological level both within its industry and in its healthcare facilities. We hope that this can be accomplished. It is sorely needed.
In the report above, I discussed the state of healthcare in the USSR as we saw it in 1990. The hospitals and care appeared to be at least thirty years behind similar Western facilities, with a lack of instruments and supplies and crumbling buildings, but with dedicated medical personnel.
At the urging of a friend, I have added a brief piece, taken from Wikipedia, about how the healthcare system in the Soviet Union (and more specifically Russia) has changed since I was there – and from the way it is described below, it really hasn’t!
Healthcare in the Soviet Union and Russia
Source: Wikipedia
Pre-reform health care
Pre-1990s Soviet Russia had a totally socialist model of health care with a centralised, integrated, hierarchically organised with the government providing free health care to all citizens. All health personnel were state employees. Control of communicable diseases had priority over non-communicable ones. On the whole, the Soviet system tended to primary care, and placed much emphasis on specialist and hospital care.
The integrated model achieved considerable success in dealing with infectious diseases such as tuberculosis, typhoid fever and typhus. The effectiveness of the model declined with underinvestment. Despite the fact that the quality of care began to decline by the early 1980s,medical care and health outcomes were on par with western standards. Despite a doubling in the number of hospital beds and doctors per capita between 1950 and 1980, the lack of money that had been going into health was patently obvious. Some of the smaller hospitals had no radiology services, and a few had inadequate heating or water. A 1989 survey found that 20% of Russian hospitals did not have piped hot water and 3% did not even have piped cold water. 17% lacked adequate sanitation facilities. Every seventh hospital and polyclinic needed basic reconstruction. Five years after the reforms described below per capita spending on health care was still a meagre US$158 per year (about 8 times less than the average European social models in Spain, the UK and Finland, and 26 times that of the U.S. which spent US$4,187 at that time).
Reform in 1991-1993
The new Russia has changed to a mixed model of health care with private financing and provision running alongside state financing and provision. Article 41 of the 1993 constitution confirmed a citizen’s right to healthcare and medical assistance free of charge. This is achieved through compulsory medical insurance (OMS) rather than just tax funding. This and the introduction of new free market providers was intended to promote both efficiency and patient choice. A purchaser-provider split was also expected to help facilitate the restructuring of care, as resources would migrate to where there was greatest demand, reduce the excess capacity in the hospital sector and stimulate the development of primary care. Finally, it was intended that insurance contributions would supplement budget revenues and thus help to maintain adequate levels of healthcare funding.
The OECD reported that unfortunately, none of this has worked out as planned and the reforms have in many respects made the system worse. The population’s health has deteriorated on virtually every measure. Though this is by no means all due to the changes in health care structures, the reforms have proven to be woefully indequate at meeting the needs of the nation. Private health care delivery has not managed to make much inroads and public provision of health care still predominates.
The resulting system is overly complex and very inefficient. It has little in common with the model envisaged by the reformers. Although there are more than 300 private insurers and numerous public ones in the market, real competition for patients is rare leaving most patients with little or no effective choice of insurer, and in many places, no choice of health care provider either. The insurance companies have failed to develop as active, informed purchasers of health care services. Most are passive intermediaries, making money by simply channeling funds from regional OMS funds to healthcare providers.
National Projects
In 2006 a national project ‘Health’ was launched to improve the country’s healthcare system through improved funding and healthcare infrastructure. This plan helped equip hospitals and clinics with advanced, high-end equipment and ambulance systems, build new medical centers, as well as launch nation-wide vaccination programs and free health checks. The project has also been working on developing medical technology market through initiatives to blend healthcare and information technology. One of the focuses was made on salary increase of medical staff working in the primary care as well as their wider training programs.
The project was initiated by the Russian President Vladimir Putin and coordinated by the Presidential administration. It was mostly financed by the federal budget. However regional and municipal levels have also contributed a lot to the financing of the program.
Reform in 2011
After Vladimir Putin became president in 2000, there was significant growth in spending for public healthcare and in 2006 it exceed the pre-1991 level in real terms. Also life expectancy increased from 1991-93 levels, infant mortality rate dropped from 18.1 in 1995 to 8.4 in 2008. Russian Prime Minister Vladimir Putin announced a large-scale health-care reform in 2011 and pledged to allocate more than 300 billion rubles ($10 billion) in the next few years to improve health care in the country. He also said that obligatory medical insurance tax paid by companies for compulsory medical insurance will increase from current 3.1% to 5.1% starting from 2011.[27] Russia, anyhow, maintains several centers of excellence, such as the Fyodorov Eye Microsurgery Complex, founded in 1988 by Russian eye surgeon Svyatoslav Fyodorov. (See my next writeup,)
This article was published in Vision Monday in August 1990.
Irving J. Arons
Arthur D. Little
I have just returned from a two week tour of four cities within the Soviet Union. I had anticipated telling you about the state of eyecare within the USSR, but unfortunately, our visit to the premier Moscow Research Institute of Eye Microsurgery was canceled at the last minute, as we were informed by Dr. Fyodorov that the “Institute will be closed in July for preventative maintenance,” and that “your visit at the term (sic) you have stated is inexpedient.” We had originally been invited following my February letter requesting to have our delegation visit the clinic. In fact, in late June we were told that we were welcome to visit the clinic, which was scheduled to shut down in August for holiday.
Apparently, the hotel we stayed at in Moscow, the Kosmos, is part of the Intourist program to provide visitors with eye care at Fyodorov’s Moscow clinic. We found a brochure advertising “Beautiful Eyes for Everybody,” and describing how the Moscow Research Institute of Eye Microsurgery “treats 22,000 people annually, restoring or improving vision and removing the need to wear eyeglasses for many.” In addition to RK (radial keratotomy), the clinic claims to do laser treatment of secondary cataract, laser treatment of glaucoma, and laser treatment of “complicated myopia of high degree.” (It must be one of the only facilities with surgical lasers in the USSR, as we visited a laser research institute and three hospitals and saw very few surgical lasers — mostly therapeutic HeNe and GaAs biostimulation type devices.)
The brochure goes on to state that your pre-operative stay is arranged at the Kosmos, and following the outpatient surgery, your post-operative treatment is done at the hotel by a team of qualified doctors and nurses. Foreign patients are offered a program of excursions, including theater tickets (the ballet only costs 4 rubles — the equivalent of 30 cents at the black market exchange rate) and other services offered by Intourist. Fyodorov hopes to treat 20,000 foreigners a year by 1992.
A recent profile of Fyodorov in Fortune (May 1989) talked about the Fyodorov entrepreneurship, with his clinic being a $75 million a year business, and growing at 30% a year annually. The clinics have over 5000 employers located at nine treatment centers across the Soviet Union, and include two factories producing eyeglasses and surgical instruments. (In addition, Dr. Fyodorov recently spent some $12 million outfitting an 11,000 ton “floating eye hospital” called the Floks, which travels from port to port in the Persian Gulf offering RK and other eye surgeries.)
Having missed out on the opportunity to visit with Dr. Fyodorov, I would like to offer some personal observations about eye care in the Soviet Union. As previously mentioned, our People-to-People delegation of medical laser specialists visited Moscow (Soviet Russia), Tblisi (Soviet Georgia), Kharkov (Soviet Ukraine), and Leningrad (back in Russia). We saw very few optical shops (none that were open) and only a small number of Soviet citizens wearing eyeglasses! One ophthalmologist at a central hospital in Kharkov told me that 50% of the people need corrective lenses — similar to the percentages in the rest of the world — but we saw very few people wearing lenses. If 5% of the people in the streets had glasses, that’s a lot. This says that Western technology and entrepreneurship could provide a needed service in the Soviet Union if a way could be found to open (and stock) optical retail shops in the major cities. However, you must remember that the average citizen only earns about 200 rubles per month (the equivalent of about $350/month at the “official” business exchange rate or about $10-15/month at the black market exchange rate of 10-15 rubles to the dollar). Therefore, the price of eyewear would have to be low for the average person to be able to afford it — unless the health care system can be convinced to reimburse or pay for the glasses. (The government health care system pays Fyodorov’s clinic the equivalent of $300 for each RK procedure carried out.)
If a Moscow McDonalds can generate hours long lines for a $5 “Big Mac”, why not $20-40 eyeglasses at a Moscow Lenscrafters or a Leningrad Pearle Vision Center?